Wearable device with AI could allow for at-home breast cancer screenings: ‘Accessible and personalized’
To provide women at a high risk of breast cancer with more frequent screenings between mammograms, researchers at the Massachusetts Institute of Technology (MIT) are developing a wearable ultrasound scanner designed to be attached to a bra.
The goal is to help women detect breast cancer tumors in the early stages and maximize the survival rate, according to a press release on MIT’s website.
The researchers’ aim was to design a wearable “miniaturized ultrasound device” that allows for “consistent placement and orientation” to take images of breast tissue, according to lead study author Canan Dagdeviren, PhD, associate professor at MIT.
WHAT IS ARTIFICIAL INTELLIGENCE (AI)?
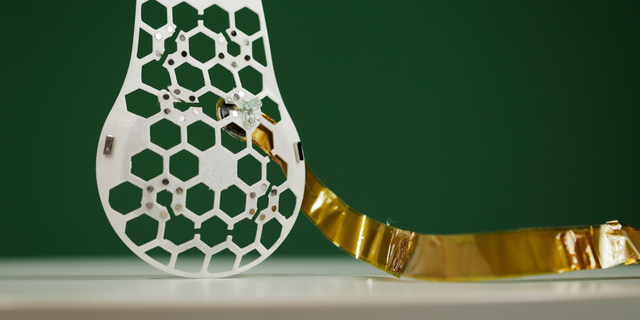
The device attaches to the bra like a patch, with a “honeycomb” pattern that has open spaces for the tracker to move through for an optimal field of view, Dagdeviren told Fox News Digital.
“The ultrasound generates a wave that penetrates the targeted breast tissue,” he said.
“When the ultrasound wave sees an obstacle like a tumor, it reflects [that] — and the ultrasound device captures this reflected wave and generates a black-and-white ultrasound image.”
He added, “From this image, you can find the coordination and shape of any anomaly in the soft breast tissue.”
AI TECH AIMS TO DETECT BREAST CANCER BY MIMICKING RADIOLOGISTS’ EYE MOVEMENTS: ‘A CRITICAL FRIEND’
In a study, a woman with a history of breast cysts wore the bra and patch, and the researchers scanned the breast at six different locations according to the patch design.

The technology recorded the images of the breast tissue, which displayed cysts as small as 0.3 centimeters in diameter — the approximate size of tumors at early stages of the disease.
The device is designed as a complement to traditional screenings by medical professionals rather than a replacement, Dagdeviren said.
“For personal health care and monitoring at home, this device can be considered as a replacement [for] the conventional handheld probe or ABUS system at the early stage of breast tumor imaging,” he said.
Researchers plan to use artificial intelligence to analyze the ultrasound images and make diagnostic recommendations.
“For breast tumor diagnosis, this device can be a strong complement to existing screening methods, making long-term breast imaging efficient and convenient.”
In the future, researchers plan to use artificial intelligence to analyze the ultrasound images and make diagnostic recommendations.
“The AI integration has the potential to enhance diagnostic accuracy through data analysis, and also holds potential for early detection and personalized care pathways for other diseases,” Dr. Harvey Castro, a Dallas, Texas-based board-certified emergency medicine physician and national speaker on AI in health care, told Fox News Digital.
Castro was not involved in the research but reviewed the details of the device.
“For breast tumor diagnosis, this device can be a strong complement to existing screening methods, making long-term breast imaging efficient and convenient.”
It could be three or four years before the device is available to consumers, Dagdeviren said.
“The critical step is the portable system and wireless communication to the hospital,” he told Fox News Digital.
NEW AI ULTRASOUND TECH IS FIRST TO LAND FDA APPROVAL TO ENHANCE PRENATAL CARE: ‘BETTER HEALTH OUTCOMES’
The company will also need to complete intensive human trials and gain FDA approval — something that Dagdeviren expects to cost around $40 million.
Dagdeviren said he does not foresee any safety risks associated with the device, as it does not use radiation.
Also, the wearable ultrasound patch can be used over and over, the release on MIT website’s noted. It could also help diagnose cancer in people who don’t have regular access to screening.
Limitations of the system
The device requires a long, flexible cable to connect the image processing system, the study’s lead author noted.
Additionally, the system that collects all of the data is currently large and stationary.

“We are currently working on a portable system, which we hope to publish in a few months,” Dagdeviren said.
The imaging resolution is “sufficient, but not superior,” he noted, and the researchers are working on various image processing methods.
“In our next paper and patent, all of these limitations will be eliminated in around six months,” Dagdeviren said.
Technology holds ‘potential to save lives’
“The development of this wearable device for breast cancer detection represents a significant advancement in health care technology,” Castro told Fox News Digital.
“Its potential to save lives and extend its promise to other diseases is immense.”
“It cannot replace traditional mammograms and other preventive care from a breast cancer expert.”
Castro added, “However, careful consideration of its implementation, including rigorous testing, alignment with existing medical protocols, and ethical considerations, will be essential to its success.”
To maximize the potential of this technology, he emphasized the need to “strike a balance between innovation and responsible medical practice.”

There is also the need to ensure the privacy and security of personal health data and to consider “potential disparities in access,” especially if the device becomes a commercial product, Castro noted.
AI BABIES: NEW TECHNOLOGY IS HELPING FERTILITY DOCS CHOOSE THE BEST EMBRYOS FOR IVF
Depending on the user’s skill level, there could also be a risk of inconsistencies and inaccuracies, he pointed out.
“It embodies the convergence of technology and health care, reflecting a future where medical care is more accessible and personalized,” Castro said.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
“However, it cannot replace traditional mammograms and other preventive care from a breast cancer expert.”
Aside from skin cancers, breast cancer is the most common cancer in U.S. women, representing one in three of all female cancer diagnoses each year, according to the American Cancer Society.
When breast cancer is caught early, the five-year survival rate is 99%. If it is detected in advanced stages, the survival rate is only 25%.
Read the full article Here


