Study on MDMA’s use to treat PTSD could send therapy method to FDA for approval by 2024
A new study published last week suggests the psychedelic drug MDMA, also known as Ecstasy or Molly, can reduce symptoms of post-traumatic stress disorder, and some expect the treatment to be approved by 2024.
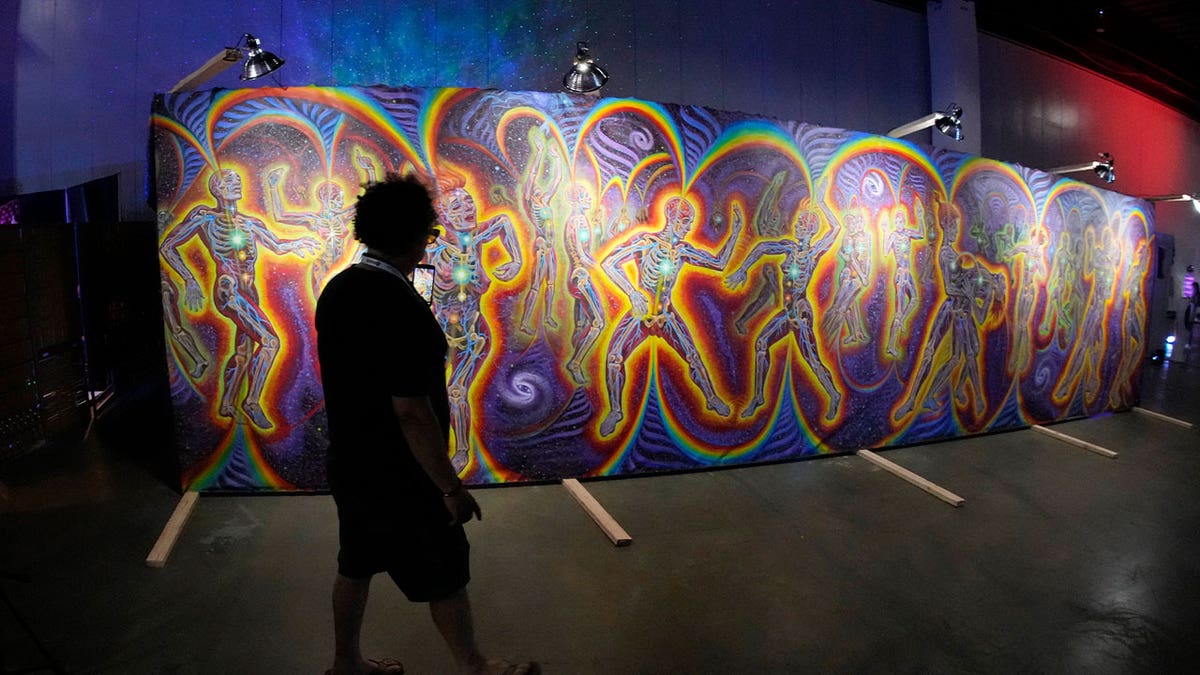
The Multidisciplinary Association for Psychedelic Studies (MAPS), a non-profit research and educational organization that was formed in 1986 and focuses on the medical, legal and cultural contexts for how people can benefit from the “careful” uses of psychedelics and marijuana, sponsored the study.
“Thanks to the combined efforts of dozens of therapists, hundreds of participants who volunteered in MAPS-sponsored trials, and many thousands of generous donors, MDMA-assisted therapy for PTSD is on track to be considered for approval by the FDA in 2024,” MAPS founder and president Rick Doblin said.
AUSTRALIA BECOMES 1ST COUNTRY TO ALLOW PATIENTS WITH DEPRESSION, PTSD TAKE PSYCHEDELICS
The results for the third phase of the study were published in Nature Medicine on Sept. 13, 2024.
During the study, researchers measured the symptoms and results of 104 people suffering from PTSD, who were randomly assigned to be prescribed MDMA or a placebo pill over the course of three sessions, one month apart. Both groups, the study notes, were given talk therapy during the process.
One person dropped out of the MDMA group during the study, and some of the side effects felt in the MDMA group included nausea, sweating, muscle tightness and a decreased appetite.
MIGRAINE NASAL SPRAY FROM PFIZER SNAGS FDA APPROVAL FOR EXPECTED SUMMER LAUNCH
A standard PTSD assessment measuring things like flashbacks, nightmares and insomnia found that 86% of the MDMA group improved, compared to 69% in the placebo group.
Once the study was complete, 72% of those in the MDMA group no longer met the criteria to be diagnosed with PTSD, compared with 48% of the people in the placebo group.
In July, Australia became the first country to allow psychiatrists to prescribe certain psychedelic substances to patients with depression or PTSD.
MIGRAINE VS. HEADACHE: HOW TO TELL THE DIFFERENCE AND WHEN TO SEEK HELP

The approval of the therapy meant Australian physicians could now prescribe doses of MDMA, while psilocybin, the psychoactive ingredient in psychedelic mushrooms, can now be given to those with hard-to-treat depression.
The U.S. Food and Drug Administration designated psilocybin as a “breakthrough therapy” in 2018, a label that’s designed to speed the development and review of drugs to treat a serious condition. Psychedelics researchers have benefited from federal grants, including Johns Hopkins, and the FDA released draft guidance late last month for researchers designing clinical trials testing psychedelic drugs as potential treatments for a variety of medical conditions.
Still, the American Psychiatric Association has not endorsed the use of psychedelics in treatment.
Medical experts in the U.S. and elsewhere, Australia included, have cautioned that more research is needed on the drugs’ efficacy and the extent of the risks of psychedelics, which can cause hallucinations.
The Associated Press contributed to this report.
Read the full article Here


