Patients have turned to ‘blood washing’ to treat long COVID
Desperate to have their lives back, long COVID patients are turning to an expensive “last resort” therapy to cure the mysterious illness.
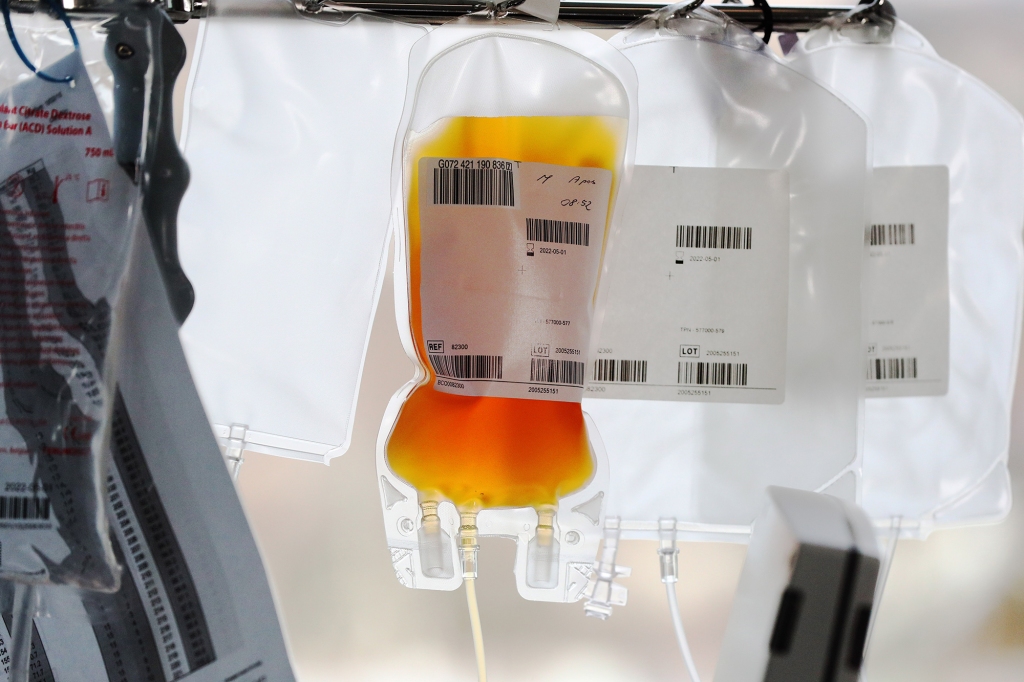
Apheresis, or “blood washing,” is a process in which a component of blood, such as plasma, is separated and then filtered back into your body via giant needles inserted into a vein.
Gitte Boumeester, who found out about “blood washing” through a Facebook support group, spent more than $15,000 to have the treatment, BMJ and ITV News reported, in a joint investigation out Tuesday.
“I thought, what’s the worst thing I’ve got to lose?” the Dutch psychiatrist-in-training told reporters. “Money was the only thing.”
And that she did — once Boumeester concluded, two months after the procedure, that the “blood washing” didn’t work.
The process is typically used in cases where it’s necessary to remove specific components of blood, such as the treatment of blood cancers, plasma and platelet donation or to collect stem cells.
But in Germany, doctors consider it one of the last resorts for the treatment of some lipid disorders, which are marked by abnormal levels of lipids, or fats, in the blood — the effects of which some have theorized are similar to long-term COVID infection.
Boumeester’s battery of tests revealed nothing about her condition, which developed soon after she caught the SARS-CoV-2 virus in November 2020, despite her debilitating exhaustion.
Yet some researchers, namely Dr. Beate Jaeger, have hypothesized that long COVID may be caused by small clots in the blood that get in the way of the flow of oxygen, leading to the telltale extreme fatigue and muscle aches. Thus, “washing” the blood of unnecessary lipids and proteins, in combination with the use of anticoagulants, blood thinners such as clopidogrel, apixaban and heparin, could help clear the capillaries for better blood circulation.
Jaeger, a cardiovascular specialist in Mülheim, Germany, fought to see apheresis used on COVID patients in the ICU and to publish a paper on her approach, attempts of which were denied. Finally, a pair of her patients agreed to undergo the treatment free of charge. Then, 60 more opted-in. She’s since seen “extremely successful” results in thousands of patients, she said.
In one of her reports, Jaeger claimed that a long COVID patient who used a wheelchair could miraculously walk again following treatment. Another improved their stride from a labored walk to a jog.
Beverley Hunt, medical director of the charity Thrombosis UK, told BMJ, “I am worried these patients have been offered therapies which have not been assessed by modern scientific methods: well-designed clinical trials. In this situation the treatment may or may not benefit them but, worryingly, also has the risk of harm.”
The process of apheresis is safe if properly performed, but there are potentially dire consequences to having overly-thin blood, particularly if hemorrhage occurs.
Even under the safest conditions, patients also risk financial ruin. Boumeester traveled some 1,700 air miles to the Long Covid Center in Larnaca, Cyprus. For two months, she rented an apartment on the beach while making weekly appointments for apheresis, and more unproven “add-on” therapies, such as hyperbaric oxygen and intravenous vitamin infusions.
Six rounds of “blood washing” cost her more than $1,600 per session, while additional treatments came with price tags up to about $150, which she did on the recommendation of the clinicians.
“I was a little ambivalent about all the extra treatment, but I promised myself if I was there I would do anything, to just try,” she said.
Experimental treatments are generally permitted throughout Europe as long as there’s clear patient consent, but experts fear that clinics like the Long Covid Center may be overpromising.
“People could potentially go bankrupt accessing these treatments, for which there is limited to no evidence of effectiveness,” said University of Birmingham researcher Shamil Haroon, whose work on the Therapies for Long Covid in Non-hospitalized Patients trial will eventually go on to inform how doctors approach the disease.
Like Boumeester, British businessman Chris Witham, from Bournemouth, traveled across the continent, to Kempten, Germany, for a $7,000 course of apheresis that didn’t work.
“I’d have sold my house and given it away to get better, without a second thought,” he told BMJ and ITV News.
The outlets spoke to just six long COVID patients who said the procedure improved some of their condition, though symptoms lingered.
Their reporting flies in the face of claims made by Austrian entrepreneur and long COVID sufferer Markus Klotz, who founded the clinic in Cyprus and claims it worked for him after having the treatment with Jaegar in Mülheim. “Over 80% of patients report to keep their gains permanently,” read one post on the Facebook page for the Apheresis Association, also led by Klotz.
“I realized before I started that the outcome was uncertain, but everyone at the clinic is so positive that you start to believe it too and get your hopes up,” Boumeester said.
Read the full article Here


