‘Remarkable’ gene-editing treatment for sickle cell disease is approved by FDA
Modern medicine is one step closer to potentially curing sickle cell disease.
On the heels of the U.K.’s authorizing the world’s first gene-edited treatment for sickle cell disease on Nov. 16, the U.S. Food and Drug Administration (FDA) approved the same treatment on Dec. 8.
“CASGEVY’s approval by the FDA is momentous,” Reshma Kewalramani, M.D., chief executive officer and president of Vertex Pharmaceuticals in Boston, said in a statement provided to Fox News Digital.
ALZHEIMER’S BLOOD TEST COULD HIT THE MARKET IN EARLY 2024, RESEARCHERS SAY
“It is the first CRISPR-based gene-editing therapy to be approved in the U.S.”
“These approvals represent an important medical advance with the use of innovative cell-based gene therapies to target potentially devastating diseases and improve public health,” said Peter Marks, M.D., Ph.D., director of the FDA’s Center for Biologics Evaluation and Research, in the agency’s press release.
“Today’s actions follow rigorous evaluations of the scientific and clinical data needed to support approval,” he also said “reflecting the FDA’s commitment to facilitating [the] development of safe and effective treatments for conditions with severe impacts on human health.”
ANTI-AGING DRUG FOR DOGS FROM SAN FRANCISCO FIRM MOVES CLOSER TO GAINING FDA APPROVAL
The CASEVY treatment — also known as exa-cel, or exagamglogene autotemcel — uses technology that “edits” the genes that cause sickle cell disease.
To develop the drug, Boston-based Vertex and CRISPR Therapeutics, which is based in Switzerland, used a gene-editing system known as CRISPR-Cas9 to turn genes on and off, according to the Sickle Cell Disease Association of America website.

“CASGEVY is a first-in-class treatment that offers the potential of a one-time transformative therapy for eligible patients with sickle cell disease,” said Kewalramani.
The inventors of the CRISPR technology won the Nobel Prize in 2020.
BLOOD CANCER AWARENESS: COMMON TYPES, SIGNS AND TREATMENT OPTIONS
CRISPR stands for “clustered regularly interspaced short palindromic repeats,” which are repetitive sequences of DNA.
“The CRISPR technology [that is] being used with this treatment for sickle cell disease — a devastating inherited illness that profoundly affects survival and quality of life — is remarkable,” Dr. Mikkael Sekeres, chief of the division of hematology of Sylvester Cancer Center at the University of Miami, told Fox News Digital.

He was not involved in the drug’s development.
“The data from the admittedly small study in support of the treatment’s approval by the FDA are impressive, and the therapy was thought safe by a panel of independent experts,” Sekeres added.
“CASGEVY is a first-in-class treatment that offers the potential of a one-time transformative therapy for eligible patients with sickle cell disease.”
The treatment is approved for people 12 and older with severe sickle cell disease who get recurrent pain syndromes known as vaso-occlusive crises, in which blood flow is blocked due to sickle cells.
The FDA also approved Lyfgenia, the first cell-based gene therapy for the treatment of sickle cell disease in people 12 years of age and older, per the agency’s press release.
What to know about sickle cell disease
Sickle cell disease is the most common inherited blood disorder in the United States, affecting an estimated 100,000 Americans, as the National Institutes of Health (NIH) noted on its website.
It disproportionately affects people of Black or African ancestry.
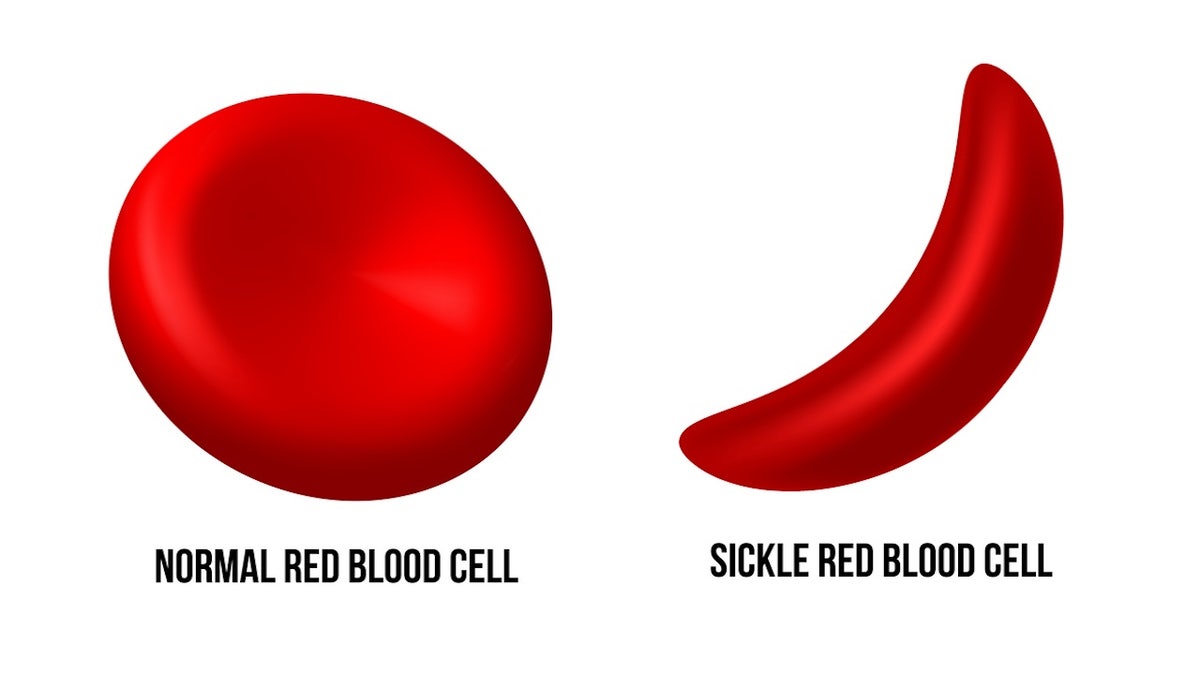
Red blood cells, which are produced in the bone marrow, contain a protein called hemoglobin that helps carry oxygen throughout the body.
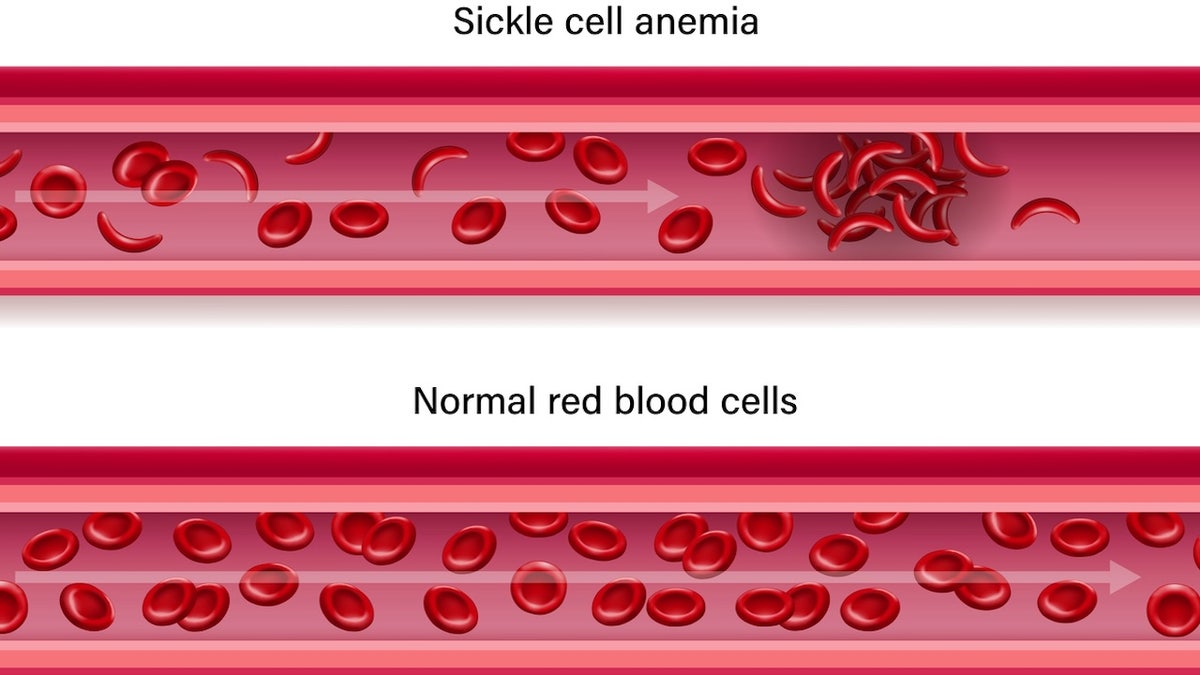
The cells are normally a round shape, which allows them to easily travel through small blood vessels, according to the Centers for Disease Control and Prevention (CDC) website.
Patients with sickle cell disease inherit a gene mutation that produces abnormal hemoglobin, which makes it more difficult for the cells to move through the bloodstream, per the NIH.
SUICIDE AND GENETICS: STUDY IDENTIFIES 12 DNA VARIATIONS THAT COULD INCREASE THE RISK
The diseased cells eventually get stuck in blood vessels, which blocks blood flow — sometimes leading to painful episodes (known as sickle cell crises), infection, acute chest syndrome or stroke, per the CDC.
The cells begin to take on the shape of the C-shaped farm tool known as a sickle, which led to the disease’s name.
How the therapy works
While in utero, fetuses make a type of hemoglobin called fetal hemoglobin, which does not cause cells to sickle and has been shown to make sickle cell disease milder in those who have it.
After a baby is born, the BCL11A gene instructs the red blood cells to stop producing fetal hemoglobin. The gene is usually turned off within six months of birth, a Vertex spokesperson told Fox News Digital.
CASEVY works by targeting — and “turning off” — the BCL11A gene.
This enables continued production of fetal hemoglobin and significantly reduces the damage from sickle cells, according to Vertex.
Although the treatment may not “cure” sickle cell disease, as patients will still have the sickle cell mutation, it could potentially eliminate most of the signs and symptoms, even if a small subset of the patient’s red blood cells continue to sickle, the Vertex spokesperson told Fox News Digital.
KIDS’ SLEEP PROBLEMS COULD BE INHERITED, NEW RESEARCH SUGGESTS
To receive the treatment, patients will undergo a bone marrow transplant.
First, the patient will receive medication to help stem cells move from the bone marrow into the bloodstream. Next, the blood will be collected and the stem cells isolated.
The cells then will be shipped to a laboratory, where genetic technology will be used to edit their DNA.

The patient will then receive chemotherapy to destroy all potential stem cells, ideally, that could produce sickle cells in the future.
The edited cells then will be infused back into the patient under the monitoring of health care professionals, who will ensure that healthy cells are produced in the bone marrow.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
The FDA recommends that patients be monitored for health issues for 15 years after treatment.
Potential limitations and cautions
More research is needed to determine the treatment’s long-term effectiveness, experts say.
It’s unclear whether the treated stem cells will continue to produce red blood cells that don’t sickle for the rest of the patient’s life, or if the cells will die off after a certain number of years, the Sickle Cell Disease Association of America cautioned on its website.
As the patients also receive chemotherapy, potential adverse effects could include infertility, secondary cancer or infectious complications.
The cost of the therapy and eligibility restrictions may also limit who can receive it.
The treatment could cost millions of dollars per patient, according to recent reports.
“The million-dollar question is how people with the disease will be able to afford this life-altering treatment, and how the health care system can sustain such costs,” Sekeres told Fox News Digital.
For more Health articles, visit www.foxnews.com/health.
Read the full article Here


