Tennessee’s lawyer Chloe Akers bewildering abortion ban
Chloe Akers considers herself a grizzled criminal defense attorney. Until a few months ago, she didn’t spend much time thinking about abortion — for all her 39 years, abortion was not a crime, so she’d never imagined having to defend someone accused of performing one.
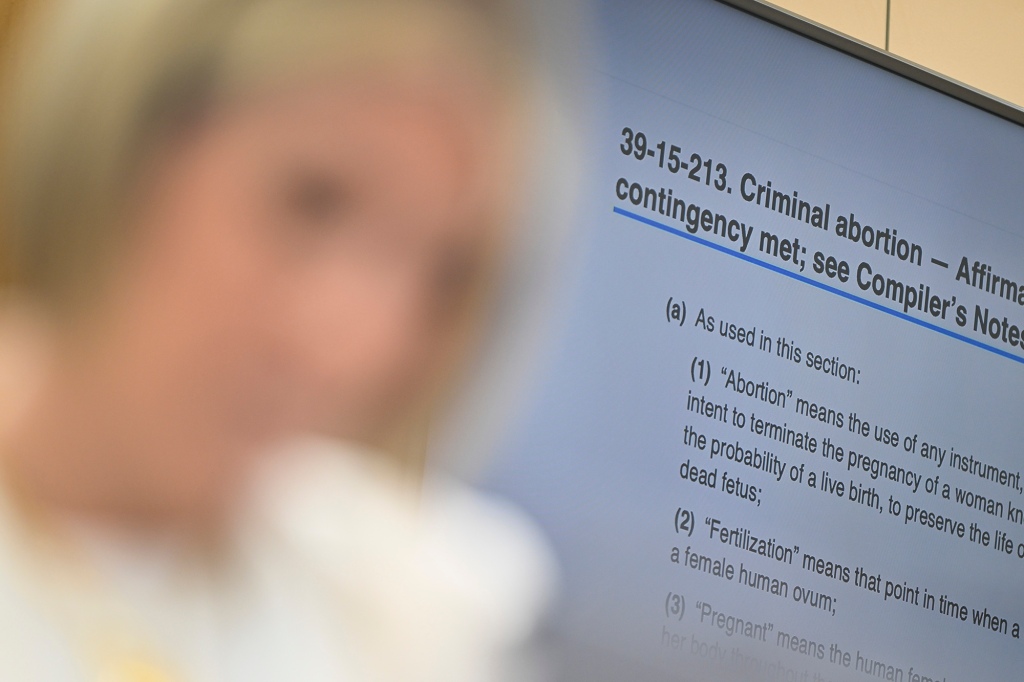
That changed in June, when the Supreme Court overturned Roe v. Wade. Akers sat down in her law office and pulled up Tennessee’s new criminal abortion statute.
She didn’t read it through a political lens; it doesn’t matter whether she likes a law — there are a lot of them she doesn’t like. Instead, she read it like she would any other statute: What does it make illegal? How would it be enforced?
She was shocked. She read it maybe 10 times more. Surely, she was missing something.
Tennessee’s law is one of the strictest in the country. It makes performing an abortion a Class C felony, punishable by up to 15 years in prison. There are no exceptions. This is the part that Akers has since found herself having to repeat, often eliciting raised eyebrows and deeply drawn breaths: Unlike many states’ abortions bans, including the one in Texas, this law does not explicitly exempt abortions performed to save a mother’s life.
Instead, it offers doctors an “affirmative defense.” The difference is linguistically subtle but extraordinarily meaningful in criminal law, Akers says. The law makes performing all abortions illegal. And instead of the state having to prove that the procedure was not medically necessary, the law shifts the burden to the doctor to convince a court that it was.
She ran down the hallway toward a colleague’s office: “Have you read this?” she gasped.
Then she opened up Instagram, where she sometimes explains criminal law to a handful of followers. She looked into the camera and explained that there are no exceptions for rape, for incest or for those so desperate they threaten to end their lives.
“Our legislature is not having any of that,” she said. “They straight-up criminalized abortion.”
If she would have known that 2 million people would end up watching her 13-minute video — including members of Congress and country music stars — she would have brushed her hair and spit out her gum.
She tried to explain an affirmative defense in a way people without a law degree might understand it: It is akin to claiming self-defense after killing someone. A prosecutor might decide the killing was justified and decide not to charge. But that’s entirely up to the prosecutor. If they do charge, the defendant is at the mercy of the courts.
“It’s about to get real, and it may not happen to you. But it’s going to happen here,” she said. For those who were scared or confused, she added words of support: “You know exactly where to find me.”
And they did. Her inbox was flooded with thousands of messages, so many she couldn’t keep up.
The mayor wrote. Socialites invited her to present at dinner parties. Doctors pleaded for guidance. A women’s motorcycle club asked her to come to talk with them.
She had accidentally become the state’s primary interpreter of this law, which went into effect Aug. 25. Within days she quit her cushy job in a law firm and started a nonprofit she named Standing Together Tennessee. For the past two months, she’s crisscrossed the state on a tour aimed at explaining this abortion law to doctors, and the intricacies of pregnancies to the lawyers who might have to defend them.
As she climbed off the stage after her latest stop at a Nashville synagogue, a doctor asked a question she’s heard again and again.
“Are they really going to enforce this?”
Akers’ answer is always the same.
“I don’t know.”
Nikki Zite, a Knoxville OB-GYN, watched Akers’ video and sent her a message.
“I need to know you,” she wrote. “I think physicians and people will be very confused about the affirmative defense. How close to dead does the patient need to be?”
Zite is a complex family planning physician, and until recently provided abortion care for pregnancies that threatened the life of the mother and for those where it was clear the fetus would not survive. The latter are no longer allowed in Tennessee.
These are often desired pregnancies, with parents who have decorated nurseries and decided on names. It’s devastating every time, she said. Since Roe fell, her colleagues had to tell three mothers carrying babies who would not survive that the law forbids them from ending their pregnancies.
She’s also treated two ectopic pregnancies, where the pregnancy is growing outside the womb, usually in the fallopian tubes. An ectopic pregnancy can never be viable and can rupture if allowed to continue to grow, threatening the mother’s life. Termination is standard treatment. And yet Zite has found herself looking over her shoulder.
“What if someone disagrees with me? Am I going to go to jail?” she wonders.
Zite is on the executive committee of the Tennessee section of the American College of Obstetricians and Gynecologists, which issued a statement that the trigger law might lead doctors to hesitate, to contact lawyers in the midst of medical emergencies, while their patients get sicker.
One day soon in Tennessee, a doctor will inevitably see a woman whose water breaks early, weeks before viability, Zite said. She will not be on her death bed, but risks infection, sepsis, bleeding.
She knows how risky delays can be: After Texas passed its six-week abortion ban last year, researchers studied 28 patients who were enduring dangerous pregnancies and hospitals interpreted the law to mean they had to delay care until the patient became sicker. More than half suffered serious health complications, twice the rate of patients in states where abortions were immediately available.
“We are now at the mercy of the criminal justice system,” Zite said. “Should I win? I think so. But do I want to go through that? No. I don’t want to feel guilty until proven innocent.”
She signed up to be the medical director of Akers’ nonprofit. They hosted a panel of doctors and asked them: What are you afraid of?
Akers can’t stop thinking about an oncologist who described a scenario pregnant women face with some regularity: They are diagnosed with aggressive cancer in early pregnancy, when they cannot receive chemotherapy or radiation.

Before, doctors would have hard conversations with patients about how they would like to proceed. They could delay treatment, understanding that their cancer might grow. Or they can terminate and treat themselves immediately, save their own lives and try for a baby once they are well.
Akers asked the doctor what they planned to do in that scenario after the trigger ban.
“That’s what we’re asking you,” the doctor said.
Akers knows pressure. Every time she speaks to a jury, her client’s freedom is on the line. Still, she said, the stakes seem higher here.
She’s lost weight. She barely sleeps. She jolts awake at night, her head spinning with questions:
What about insurance companies? If termination is illegal, even to save a mother’s life, will they pay for it? Would that make them an accomplice akin to a getaway driver?
What about nurses? Anesthesiologists?
Providers must submit a form to the state reporting every termination. Now, would that amount to forcing them to prepare evidence against themselves in violation of the constitution’s protection against self-incrimination?
“It’s like I opened a box, and thought there was one question. And in answering that question, 10 more questions arise and 10 more from that and 10 more from that,” she said. “That’s the most frustrating part about this whole endeavor is feeling like I’m on a merry-go-round, going round and round.”
When she first began her tour, she thought of it as a pragmatic, apolitical effort to explain the law without the fervor of the abortion wars. She’d leave the debate to others.
But she’s grown indignant about the confusion that continues to swirl over what the law really says. Many, including legislators who passed it, insist it includes an exemption to save the mother’s life.
“I don’t know how many other ways to say there’s no exceptions. We can’t tell people that it’s not going to be prosecuted,” Akers said. “People might be like, ‘Why is this lady being so persnickety and detail-oriented?’ Because I’m a lawyer.”
Words matter in a courtroom. She’s spent hours arguing with prosecutors over the definition of “unreasonable.” There is no world in which she can imagine telling a judge that her client thought there was an exception, even though there wasn’t.
As a criminal defense lawyer for 15 years — many of them as a public defender — she’s well acquainted with the mercilessness of America’s criminal justice system.
“I think there is this hope in people. That because this is so unreasonable and because this is so antithetical to what we think of as fair and just and American, that they’re like, surely, surely someone’s not going to prosecute this. Right?” she said. “But I have seen cases that would make your skin crawl.”
She’s watched the courts throw the book at mentally ill clients, homeless veterans, children, people struggling with addiction.
So she told the doctors in Nashville:
“Do I suspect that this law will be enforced? Yes, I do. Otherwise, why write laws?”
Will Brewer, an attorney and lobbyist with Tennessee Right to Life, thinks the lawyers like Akers and doctors agonizing over the wording are exaggerating the possible consequences.
“I think you’re going to be hard-pressed to find a prosecutor that is going to prosecute a physician when they can back up their claim that they did this to save the life of the mother,” Brewer said.
Brewer has said — and has written in published essays — that the law should be interpreted as only applying to elective abortions, when the sole reason for termination is that the mother doesn’t want a baby.
Yet he said lawmakers chose the wording for a specific reason: to raise the bar high for doctors to perform an abortion. Exemptions are easier to abuse, he said. It was designed to be a narrow window where abortions would be justified.
The law mandates doctors prove only that the abortion in their “good faith medical judgment” was necessary “to prevent the death of the pregnant woman or to prevent serious risk of substantial and irreversible impairment of a major bodily function.”
That gives them wide berth, Brewer thinks — it doesn’t require death be imminent and it doesn’t mean every decision will be second-guessed.

“You still end up in the same place at the end of the day,” he said of the line between an exemption and a defense. “But you just make sure the due diligence was done and that the law was treated with the seriousness that it deserves.”
He pointed to Ohio laws in effect for years that used affirmative defense language in banning later-term abortions except in medical emergencies.
“Were any physicians charged with violating any of these laws? No, not one,” he said.
That no one was prosecuted because of them does not reflect the true toll they have taken on doctors, said Danielle Bessett, a professor at the University of Cincinnati. She held focus groups with 35 Ohio physicians working in hospitals and private practice, not abortion clinics.
Doctors reported feeling demonized, confused, powerless. They described waiting to perform an abortion they knew would be inevitable until the patient became sicker so the hospital would deem their condition “bad enough.” Others said they advised patients to go out of state for terminations if they were in decent health to travel.
Pregnancy complications are not black-and-white, Bessett said. It was cases in the gray area, where serious health consequences were not imminent but likely, that caused doctors “great moral distress,” Bessett said.
And these Ohio laws governed only later-term abortions, which account for a tiny fraction of terminations, she said. The post-Roe laws like the one in Tennessee will govern virtually all pregnancies, so the number of times a termination could be questioned in court will skyrocket.
Idaho has a trigger ban nearly identical to Tennessee’s. The wording is the same, though unlike Tennessee’s, it includes an affirmative defense for rape or incest. And while Tennessee’s includes one to protect the mother from death or serious injury, Idaho’s scraps the language about injury and allows an abortion only to prevent death.
The United States Department of Justice sued that state, arguing that the ban would force hospitals to violate federal law that requires they stabilize patients in medical emergencies.
U.S. District Judge B. Lynn Winmill blocked part of the ban from taking effect.
Lawyers representing the state had argued in part that in the “real world,” no prosecutors would ever bring charges against a doctor for performing an abortion on a sick patient.
Winmill seemed skeptical. They were asking him to ignore what the law actually says, he wrote. It makes criminal what doctors routinely do to care for patients. One gynecologist had described for the court that physicians were “bracing for the impact of this law, as if it is a large meteor headed towards Idaho.”
“More fundamentally,” Winmill wondered, “if the law does not mean what it says, why have it at all?”

Akers was on her way home from the Nashville stop on her speaking tour when another doctor called for help. Leilah Zahedi, a Chattanooga OB-GYN, said she’d been on a conference call with hospital lawyers who reminded her that if she hesitates too long and a pregnant patient suffers, she could be liable for malpractice.
“We’re being told there’s this very fine tightrope where you can follow the law. And if you fall one way, you’re committing a felony and if you fall the other way and you wait too long, then someone can sue you for malpractice. It feels pretty much impossible,” she said. “What am I supposed to do?”
She specializes in the most dangerous pregnancies. Complications uncommon for most obstetricians are not uncommon for her. She wants to stay in Tennessee, but she’s not sure if the new law will make that too risky.
“The women of Tennessee need you here,” Akers said. This is her greatest fear: Doctors will move to states where they will not face the threat of jail for doing their jobs.
Akers’ own sister survived a high-risk pregnancy with twin boys — because she had top-notch care, she believes. She thinks all of her neighbors deserve the same. One of her closest friends, a lifelong Republican and fellow lawyer, recently gave birth after a high-risk pregnancy. She’d thought she’d have more children, but now, because of the law, she fears getting pregnant again.
Tennessee already ranks toward the top of the list of states with abysmal maternal mortality rates, and Zahedi worries this will make matters worse.
Soon after Roe was overturned, a patient was referred to Zahedi. She’d had two uncomplicated pregnancies before, delivered by Cesarean section. But this time her water broke early at 15 weeks. The likelihood of the baby surviving birth was extremely low; without fluid, a baby’s lungs will not develop.
Some such patients choose to keep their pregnancies and risk their own health to be able to hold their babies for the few moments they are alive. Others choose to terminate. Zahedi helps them either way. It is a personal choice, she believes, and not one she or anyone else should make for them.
Then Zahedi discovered a dangerous complication: the woman’s placenta was growing into her C-section scar and her uterus. It could cause severe infection and bleeding, and she’d likely lose her uterus.
The patient, a woman of strong faith, agonized over the choice, and Zahedi lived through that grief and despair alongside her. The patient didn’t want to risk leaving her two living children motherless and decided to terminate.
Zahedi didn’t sleep the night before the procedure. She was worried for her patient, and for herself.
“We all just risked our lives for two years in a pandemic. I’m not really excited about now risking my liberty and freedom in order to take care of patients here when it has become very clear I am no longer welcome,” she said, “even though I know people need me.”
She wants to stay. She loves her practice and her patients, she told Akers.
“But I just don’t know.”
Akers sighed as they hung up, and shook her head. She gets calls like this from doctors all the time now.
She hopes she’s wrong and making a big deal out of nothing. Maybe none of them will be prosecuted; maybe the intent was only to shut down abortion clinics. If a year from now, all is well, she’ll happily fold her new nonprofit and go back to defending people charged with other crimes.

“But I just keep coming back to asking, if it was really just about shutting down clinics, why not write a law that criminalized elective abortions?” she said. “If this was all just a scare tactic, well played, mission accomplished, we’re all scared. And these are situations where moments matter.”
That evening, back in Nashville, Dr. Nancy Lipsitz was working an emergency shift.
Appearing that afternoon with Akers, the gynecologist had described the fear she’s seen in her patients. One is planning to move out of state. Another asked her: If things go bad, will you have to let me die?
She feels like practicing medicine has become a minefield of risk. She struggled to find a word to describe the thought of facing criminal charges for treating patients. It was “mind-bending,” she said.
That very night, a pregnant woman came into the emergency room in extraordinary pain, with signs of internal bleeding. Lipsitz found that she had a ruptured ectopic pregnancy.
This was the very mind-bending scenario she had described from the stage just hours before, one that might have pitted the vagaries of a statute against a patient’s welfare.
Lipsitz did not hesitate. She went to work.
Read the full article Here


